Overactive bladder (OAB) is a prevalent and often distressing condition characterized by a sudden, uncontrollable urge to urinate. It signifies a significant concern within the healthcare landscape due to its substantial impact on individuals’ daily functions, overall health, and quality of life. Both men and women across various age groups may experience OAB, with its prevalence increasing with age. According to the Urology Care Foundation, approximately 33 million Americans are affected by OAB, showcasing its widespread nature.
Globally, the statistics are equally concerning. Studies suggest that OAB affects around 12-17% of the population worldwide. Notably, this condition can lead to emotional and psychological distress, with affected individuals often altering their daily routines to manage symptoms. For example, they may avoid social activities or plan their schedules around bathroom breaks, leading to a significant reduction in their quality of life.
OAB’s impact is not limited to a specific demographic, affecting both the young and elderly, though it is more common among older adults. The prevalence of OAB increases with age; nearly 30% of men and 40% of women experience symptoms at some point in their lives. Nevertheless, despite its commonality, many individuals are hesitant to seek medical help due to embarrassment or the misconception that it is an inevitable part of aging.
The importance of understanding OAB extends beyond personal health as it also strains healthcare systems. Managing OAB involves not only treating the symptoms but also addressing the psychological and social implications. For more comprehensive information on OAB, readers can refer to resources provided by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the American Urological Association (AUA).
In summary, overactive bladder is a significant health concern affecting millions globally. Understanding its prevalence, impact, and demographic reach is crucial in addressing the condition effectively and improving the quality of life for those affected.
Causes
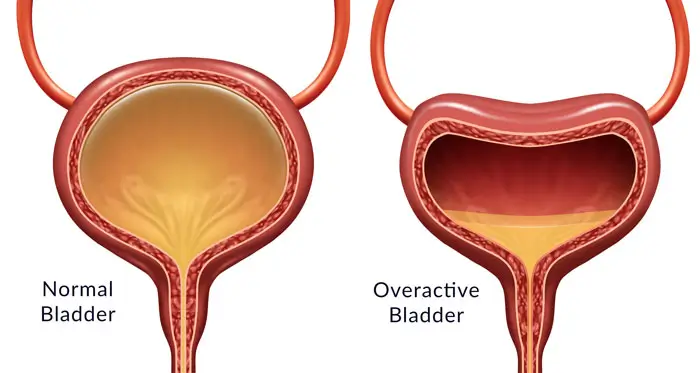
Overactive Bladder (OAB) is a condition characterized by a sudden and involuntary contraction of the bladder muscles, leading to an urgent need to urinate. Understanding the underlying causes is crucial for effective management and treatment. The primary causes of OAB can be broadly categorized into genetic, neurological, and lifestyle factors.
One significant contributor to OAB is genetic predisposition. Research indicates that individuals with a family history of overactive bladder are at a higher risk of developing the condition themselves. This suggests a genetic link, although the exact genetic markers associated with OAB are still being studied.
Neurological factors also play a crucial role in the onset of OAB. Any condition that affects the nervous system can potentially disrupt the normal communication between the bladder and the brain. This includes diseases such as Parkinson’s disease, multiple sclerosis, stroke, and spinal cord injuries. These conditions can impair nerve signals and lead to involuntary bladder contractions.
In addition to genetic and neurological causes, various lifestyle factors significantly impact the development of OAB. These include:
- Diet: Consumption of certain foods and beverages, such as caffeine, alcohol, and spicy foods, can irritate the bladder and exacerbate symptoms.
- Hydration: Both excessive fluid intake and insufficient hydration can contribute to OAB symptoms.
- Obesity: Extra weight can pressure the bladder, leading to increased urgency and frequency.
- Smoking: Nicotine can irritate the bladder lining and worsen OAB symptoms.
- Lack of physical activity: A sedentary lifestyle can weaken bladder muscles, increasing the risk of OAB.
Understanding these factors can help individuals manage their condition more effectively. For more information on related aspects of OAB, consider exploring the Symptoms and Management sections.
Symptoms
Overactive Bladder (OAB) is characterized by a series of distressing symptoms that can significantly impact an individual’s quality of life. Understanding these symptoms can aid in recognizing the condition early and seeking appropriate medical intervention. The most common symptoms of OAB include urgency, frequency, nocturia, and incontinence. Each of these symptoms manifests uniquely, necessitating a deeper exploration.
Urgency: Urgency is defined as a sudden, overwhelming need to urinate, often perceived as difficult to postpone. This symptom can occur without warning and may lead to an uncomfortable and urgent rush to the bathroom. It significantly disrupts daily activities and can lead to embarrassment and anxiety.
Frequency: Frequency refers to the need to urinate more often than what is considered normal. While the average person urinates between 6-8 times a day, individuals with OAB may find themselves going much more frequently, often requiring bathroom visits multiple times within an hour. This excessive frequency can be particularly disruptive during work or social interactions.
Nocturia: Nocturia is the need to wake up during the night to urinate. This symptom results in disrupted sleep patterns, leading to fatigue and decreased overall well-being. For those with OAB, nocturia can occur multiple times a night, severely affecting sleep quality and daytime alertness.
Incontinence: Incontinence, specifically urgency urinary incontinence, is another hallmark symptom of OAB. This involves the involuntary loss of urine following a strong urge to urinate. It can range from occasional leaks to more severe cases where larger amounts of urine are lost. This symptom can be a significant source of distress and embarrassment, impacting life quality. Discover more about incontinence.
Recognizing these symptoms early and accurately can lead to more effective management strategies, thereby improving individuals’ well-being and daily functionality.
Diagnosis
The diagnosis of an Overactive Bladder (OAB) involves a multifaceted approach to comprehensively understand and identify the condition. Physicians employ a combination of detailed patient history assessments, physical examinations, and specialized diagnostic tests to confirm the presence of OAB and rule out other underlying causes.
Initially, a detailed patient history is crucial. This involves gathering information about urinary symptoms, frequency, urgency, and incontinence episodes. Patients are often asked to maintain a bladder diary to record all urinary habits, which provides valuable insight into symptom patterns and triggers. Alongside questioning, a thorough physical examination particularly focuses on the abdomen and pelvic region to detect any anatomical abnormalities or signs of infection that could mimic OAB symptoms.
To further refine the diagnosis, several diagnostic tests may be employed:
- Urodynamic Studies: These are crucial in assessing how well the bladder and urethra store and release urine. By measuring bladder pressure and volume paired with flow rates, urodynamic tests provide detailed insights into the bladder’s functionality and any involuntary muscle contractions indicative of OAB.
- Urinalysis: This simple test helps detect blood, infections, or other abnormalities in the urine, ensuring that symptoms are not the result of a urinary tract infection or hematuria.
- Cystoscopy: This procedure involves using a small camera to visually inspect the bladder and urethra, identifying any structural issues or malignancies contributing to the patient’s symptoms.
- Postvoid Residual (PVR) Volume Test: By measuring the amount of urine left in the bladder after voiding, the PVR test can identify issues with bladder emptying, differentiating between OAB and other conditions like bladder outlet obstruction.
Employing these diagnostic tests and procedures allows for a meticulous assessment of OAB, facilitating an accurate diagnosis and aiding in developing a customized management strategy. For more information on the causes and symptoms of OAB, refer to the Causes and Symptoms sections.
Treatment
The management of overactive bladder (OAB) involves a range of treatment options designed to alleviate symptoms and improve quality of life. The choice of treatment depends on the severity of symptoms, the underlying cause, and the patient’s overall health. Treatment options are generally categorized into medical treatments, surgical interventions, and other ancillary therapies. Understanding the different approaches can help patients and healthcare providers make informed decisions.
Medical Treatments
Pharmacological treatments are often the first line of therapy for OAB. These include:
- Antimuscarinics: Medications such as oxybutynin and tolterodine work by blocking specific receptors in the bladder, thereby reducing urgency and frequency.
- Beta-3 Agonists: Mirabegron is a newer class of medication that relaxes the bladder muscle, aiding in increased storage capacity and reducing the sensation of overactivity.
These medications are generally effective, but they may come with side effects such as dry mouth, constipation, or blurred vision, which should be discussed with a healthcare provider.
Surgical Options
When pharmacological treatments are insufficient, surgical interventions may be considered. These include:
- Bladder Augmentation: A procedure where segments of the intestine are used to enlarge the bladder, which can help reduce the severity of symptoms. However, this is usually reserved for severe cases.
- Neuromodulation: This therapy involves electrical stimulation of nerves that control bladder function. Devices such as sacral nerve stimulators can be implanted to help manage symptoms.
These surgical options are typically considered when other treatments have failed, and they require thorough discussion with a urologist to weigh the benefits and risks.
Other Interventions
Besides standard medical and surgical treatments, other interventions can also be beneficial:
- Pelvic Floor Muscle Training: Techniques such as Kegel exercises strengthen the muscles that control urination, offering a non-invasive solution for symptom management.
- Behavioral Therapies: Bladder training and timed voiding can be effective strategies to increase the time between voiding and reduce urgency.
Complementary therapies such as biofeedback and acupuncture are also gaining recognition for their potential benefits.
Prevention of Overactive Bladder (OAB)
Preventing overactive bladder (OAB) or mitigating its symptoms can significantly enhance one’s quality of life. While certain risk factors such as age or underlying medical conditions cannot be altered, lifestyle adjustments, dietary changes, and specific exercises can contribute to bladder health. By following recommended strategies, individuals can actively work towards reducing the onset or severity of OAB symptoms.
Implementing healthy lifestyle changes is a fundamental step in preventing OAB. Regular physical activity helps maintain a healthy weight, reducing pressure on the bladder. Additionally, avoiding tobacco and moderating alcohol consumption can play a crucial role in bladder health. Smoking can irritate the bladder and increase the risk of bladder cancer, whereas excessive alcohol intake can exacerbate bladder overactivity.
Dietary adjustments are equally critical in managing bladder health. Certain foods and beverages are known to irritate the bladder and should be consumed in moderation or avoided. These include:
- Caffeine: Found in coffee, tea, and some soft drinks, it can increase bladder activity.
- Alcohol: Can act as a diuretic, leading to increased urine production.
- Spicy foods: These can irritate the bladder lining, exacerbating symptoms.
- Citrus fruits: While healthy, their high acidity can provoke bladder irritation.
- Artificial sweeteners: These can trigger bladder contractions and should be limited.
Engaging in exercises specifically designed to strengthen pelvic floor muscles, such as Kegel exercises, can be particularly beneficial in preventing OAB. These exercises help bolster the muscles that support the bladder, thereby improving bladder control. Regular practice of Kegel exercises can lead to measurable improvements over time.
Proper fluid intake is also essential. It is a common misconception that reducing water intake can prevent frequent urination. However, inadequate hydration can lead to concentrated urine, which is more likely to irritate the bladder. The goal should be to maintain a balanced intake, ensuring enough fluids to stay hydrated without overburdening the bladder.
Adopting these preventive measures can serve as an effective strategy for managing bladder health and reducing the risk of developing an overactive bladder. For those already experiencing symptoms, these adjustments can provide considerable relief and improve daily life. For more detailed information on symptoms and diagnosis, you can explore the Symptoms and Diagnosis section.
Complications
Overactive Bladder (OAB) can significantly affect an individual’s overall health and quality of life if not managed properly. One of the primary complications that can arise from OAB is the increased risk of urinary tract infections (UTIs). The frequent and urgent need to urinate can lead to incomplete emptying of the bladder, which provides a conducive environment for bacteria to grow, thereby increasing the likelihood of developing infections. UTIs can cause symptoms such as pain, burning during urination, and even more severe complications if the infection spreads to the kidneys.
Another notable complication is the potential for skin issues. Those suffering from OAB may experience episodes of incontinence, leading to moist environments around the genital area. Prolonged exposure to dampness can result in skin irritation, rashes, and even more severe conditions like pressure sores or infections if not addressed promptly. It is vital to maintain good hygiene and use appropriate skincare products to prevent such skin issues.
The impacts of OAB are not limited to physical health; mental health can also be severely affected. The persistent worry about having an accident or the embarrassment of dealing with frequent bathroom trips can lead to significant stress and anxiety. This constant state of concern may cause individuals to withdraw from social activities and lead to isolation, which can further contribute to the development of depression and a decline in overall mental well-being. The psychological burden of OAB underscores the importance of seeking professional help to manage both the physical and emotional aspects of the condition.
Overall, the complications associated with OAB can profoundly impact day-to-day life. Proper management and treatment are crucial to mitigate these risks and improve quality of life.
Management and Lifestyle
Managing overactive bladder (OAB) requires a multi-faceted approach that integrates lifestyle changes and daily strategies to significantly improve health outcomes. By making adjustments to diet, exercise, and stress management, individuals can alleviate symptoms and enhance overall well-being.
First and foremost, dietary modifications can play a crucial role. It’s advisable to limit the intake of bladder irritants such as caffeine, alcohol, spicy foods, and acidic fruits, which can exacerbate OAB symptoms. Instead, focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins that support overall health.
Regular physical activity is another key component in managing OAB. Engaging in exercises such as walking, swimming, or cycling can improve bladder function and decrease the urgency and frequency of urination. Pelvic floor exercises, often known as Kegel exercises, are particularly beneficial as they strengthen the muscles responsible for bladder control.
Stress management is equally important, as anxiety and stress can worsen OAB symptoms. Incorporating relaxation techniques such as deep breathing, meditation, and yoga can help manage stress levels and consequently reduce OAB flare-ups.
Additionally, adopting practical coping strategies can help manage the day-to-day challenges of OAB:
- Keep a bladder diary to track fluid intake, urination times, and any triggers that may worsen symptoms.
- Establish a regular bathroom schedule. Using the restroom at planned intervals can help maintain bladder control.
- Ensure easy access to bathrooms, especially in workplaces and public settings, to reduce anxiety and discomfort.
- Utilize incontinence products such as pads or absorbent underwear for extra confidence and protection during flare-ups.
These management tips, combined with medical advice from healthcare providers, can enhance the quality of life for individuals with OAB, making it possible to lead an active and fulfilling lifestyle.
Research and Innovation
The landscape of overactive bladder (OAB) management is evolving, thanks to ongoing research and innovation. Recent advancements have introduced new therapeutic options and technologies that promise to enhance patient outcomes and quality of life. This section highlights some of the promising developments in the field.
One of the significant strides in OAB treatment is the development of beta-3 adrenergic agonists. These medications work by relaxing the bladder muscle, thereby reducing the symptoms associated with overactive bladder. Mirabegron, a beta-3 adrenergic agonist, has shown noteworthy results in clinical studies, offering an alternative to antimuscarinics, which often come with troubling side effects.
Another exciting development is the application of electrical stimulation therapies. Techniques such as sacral neuromodulation and percutaneous tibial nerve stimulation have demonstrated efficacy in reducing OAB symptoms. These minimally invasive procedures modulate the neural pathways responsible for bladder control, providing patients with significant relief from urgency and incontinence.
Furthermore, advances in regenerative medicine are opening new frontiers. Stem cell therapy is being explored as a potential treatment for OAB. Early studies indicate that stem cells could help repair and regenerate damaged bladder tissues, although more research is needed to establish the long-term safety and efficacy of this approach.
The integration of digital health technologies into OAB management marks another innovative leap. Smartphone applications and wearable devices are being developed to monitor bladder activity and provide real-time feedback to patients. These tools can assist in personalized treatment plans and improve adherence to therapy.
Other notable advancements include:
- Genetic research exploring the hereditary basis of OAB, could lead to more targeted therapies.
- Novel drug delivery systems that increase the efficacy and reduce the side effects of existing medications.
- Research into the role of gut microbiota in bladder function, paving the way for probiotic-based treatments.
Conclusion
Understanding overactive bladder (OAB) is crucial, as it affects many individuals worldwide and can significantly impact daily life. Early detection of OAB symptoms—such as urgency, frequency, and nocturia—is essential in managing the condition effectively. Recognizing these signs early can lead to timely interventions that improve quality of life.
Effective management of OAB typically involves a combination of lifestyle adjustments, behavioral therapies, and, when necessary, medical treatments. Simple changes such as reducing the intake of bladder irritants, practicing pelvic floor exercises, and timed voiding can make a significant difference. For more advanced cases, medications and surgical options offer additional relief. It is imperative to consult healthcare professionals to tailor a management plan that best suits individual needs and symptoms.
Preventive strategies play a vital role in minimizing the risk of developing OAB. Maintaining a healthy weight, staying physically active, and avoiding excessive caffeine and alcohol intake can help preserve bladder health. Regular check-ups and discussions with healthcare providers about any urinary concerns can also prevent the progression of symptoms and promote early intervention.
A proactive approach to bladder health includes understanding potential triggers and employing effective management techniques. Readers are encouraged to adopt these practices and seek professional advice to address any concerns promptly. For a comprehensive overview of causes, symptoms, and detailed management strategies, readers can refer to the dedicated sections on these topics within this article.